Auscultation of the lungs is a cornerstone of the respiratory examination, providing invaluable insights into the health of the airways and lung parenchyma. This non-invasive, cost-effective technique allows clinicians to assess airflow dynamics within the tracheobronchial tree and differentiate between normal and abnormal respiratory sounds. Mastering the art of lung auscultation is crucial for accurate diagnosis and management of various respiratory disorders. This guide will delve into the principles of lung sound auscultation, focusing on where to listen to various normal and abnormal sounds to enhance diagnostic accuracy.
Physics and Mechanisms of Breath Sounds
Understanding the physics of sound generation and transmission is essential for effective auscultation. Breath sounds are characterized by their frequency, intensity, and timbre, which are influenced by the airflow patterns and the structures through which the sound waves travel.
Frequency, Pitch, and Amplitude
Frequency, measured in Hertz (Hz), represents the number of sound waves per second. Pitch is the subjective perception of frequency. The human ear can detect sounds ranging from 20 to 20,000 Hz. Amplitude relates to the energy of sound waves and is perceived as loudness, measured in decibels (dB).
Timbre and Quality
Timbre, or quality, distinguishes sounds with similar pitch and loudness. It is determined by the combination of fundamental frequency and overtones (harmonics). These characteristics are crucial for differentiating various breath sounds and adventitious sounds.
Airflow Dynamics and Sound Production
Normal breath sounds are generated by turbulent and vorticose airflow within the airways. Laminar airflow, which is silent, occurs in smaller airways and at low flow rates. Turbulent flow, in contrast, is chaotic and produces sound as air molecules collide with each other and the airway walls. Vortices, or whirlpools, also contribute to sound generation, particularly in the medium-sized bronchi (5th to 13th generations).
Figure 1: Illustrating laminar flow pattern in airways.
Figure 2: Depicting Poiseuille’s equation governing laminar flow.
Figure 3: Showing turbulent airflow pattern in airways.
The sound generated within the lungs undergoes filtering by the lung parenchyma and chest wall, which act as a low-pass filter. This filtering effect attenuates high-frequency sounds, resulting in the breath sounds heard over the chest wall being predominantly low-frequency.
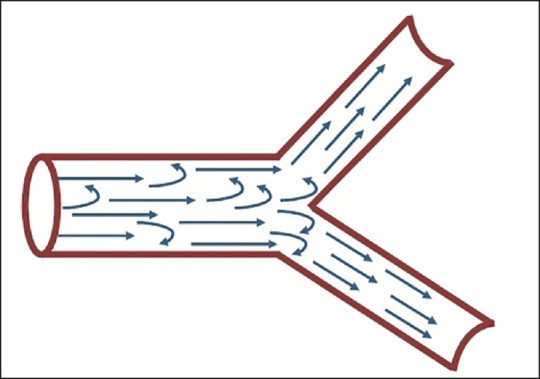 Figure 4
Figure 4
Auscultation Technique: Best Practices for Optimal Sound Detection
To accurately auscultate lung sounds, a systematic approach in a quiet environment is essential.
- Patient Positioning and Preparation: The patient should ideally be seated upright. If this is not possible, lateral decubitus positions can be used, ensuring examination of both sides of the back. The chest should be exposed, and auscultation should never be performed over clothing.
- Stethoscope Use: Warm the stethoscope diaphragm by rubbing it in your hands. Use the diaphragm for listening to breath sounds as it is better for transmitting high-pitched sounds.
- Breathing Instructions: Instruct the patient to breathe deeply through an open mouth, ensuring adequate airflow for sound generation.
- Systematic Auscultation Pattern: Begin auscultation anteriorly at the apices of the lungs, moving downwards. Repeat the process posteriorly, starting from the apices and moving down. Compare symmetrical points on each side to identify any unilateral abnormalities. Listen to at least one full respiratory cycle at each location.
Where to Listen for Normal Breath Sounds
Normal breath sounds are categorized into vesicular, bronchial, bronchovesicular, and tracheal sounds, each with distinct characteristics and auscultation locations.
Vesicular Breath Sounds: Peripheral Lung Fields
Vesicular breath sounds are the most commonly heard normal breath sounds.
Where to Listen: Vesicular breath sounds are best auscultated over the peripheral lung fields. This includes the majority of the anterior and posterior chest wall, particularly in areas away from the trachea and major bronchi. Specific locations include:
- Anterior Chest: Below the clavicles and throughout the chest, laterally to the mid-axillary line.
- Posterior Chest: Between the scapulae (interscapular region) and below the scapulae, extending laterally.
- Lateral Chest: Mid-axillary lines.
Characteristics:
- Soft, low-pitched, and rustling quality.
- Inspiratory phase is longer than the expiratory phase (I:E ratio of approximately 2:1).
- Inspiration is louder and higher pitched than expiration.
- No pause between inspiration and expiration.
 Figure 5
Figure 5
Variations in Vesicular Breath Sounds:
- Exaggerated (Puerile): Louder vesicular sounds, normal in children and thin individuals, or in areas compensating for reduced function elsewhere.
- Diminished or Absent: Reduced intensity due to shallow breathing, airway obstruction, hyperinflation, pneumothorax, pleural effusion, or obesity.
- Prolonged Expiration: Normal vesicular sounds with an extended expiratory phase, often seen in obstructive lung diseases like asthma and chronic bronchitis.
Bronchial Breath Sounds: Over the Trachea and Manubrium
Bronchial breath sounds are normally heard over the larger airways.
Where to Listen: Bronchial breath sounds are physiologically auscultated over the trachea (anterior neck) and the manubrium (upper sternum) anteriorly, and between the C7 and T3 vertebrae posteriorly (over the main bronchi).
Characteristics:
- Loud, hollow, and high-pitched.
- Expiratory phase is longer than the inspiratory phase (I:E ratio reversed to approximately 1:2).
- Distinct pause between inspiration and expiration.
 Figure 6
Figure 6
Abnormal Bronchial Breath Sounds: The presence of bronchial breath sounds in peripheral lung fields indicates consolidation, pleural effusion (above the effusion level), pulmonary fibrosis, or lung collapse where the consolidated segment is in contact with the chest wall.
- Tubular: High-pitched bronchial sounds associated with consolidation, fibrosis, or pleural effusion.
- Amphoric: Low-pitched bronchial sounds with metallic overtones, heard over large cavities (e.g., pneumothorax, large lung cavity).
- Cavernous: Low-pitched bronchial sounds heard over lung cavities like abscesses or bronchiectatic cavities.
Bronchovesicular Breath Sounds: First and Second Intercostal Spaces and Interscapular Area
Bronchovesicular breath sounds are a blend of vesicular and bronchial sounds.
Where to Listen: Normally heard in the 1st and 2nd intercostal spaces anteriorly and between the scapulae posteriorly. These locations represent areas where larger and smaller airways are in proximity.
Characteristics:
- Intermediate intensity and pitch.
- Inspiratory and expiratory phases are of equal duration.
Bronchovesicular sounds heard in other locations are considered abnormal and may indicate underlying pathology.
Tracheal Breath Sounds: Over the Trachea
Tracheal breath sounds are the loudest and harshest normal breath sounds.
Where to Listen: Auscultated directly over the trachea in the anterior neck.
Characteristics:
- Harsh, very loud, and high-pitched.
- Inspiratory and expiratory phases are equal in duration with a distinct gap between them.
Tracheal sounds are not routinely assessed in peripheral lung fields but are valuable in evaluating upper airway obstruction. Changes in tracheal sounds can indicate conditions like tracheal stenosis or upper airway obstruction.
Where to Listen for Adventitious (Abnormal) Lung Sounds
Adventitious sounds are additional sounds superimposed on normal breath sounds. They are crucial indicators of respiratory pathology.
Crackles (Rales): Primarily Inspiratory, Location Varies
Crackles are discontinuous, explosive, non-musical sounds, often heard during inspiration.
Where to Listen: The location and timing of crackles can provide diagnostic clues:
- Fine Crackles (Late Inspiratory): Typically heard in the lung bases in conditions like interstitial lung disease (e.g., idiopathic pulmonary fibrosis), early congestive heart failure, and pneumonia resolution. They are often described as sounding like Velcro being pulled apart.
- Coarse Crackles (Early Inspiratory): Heard in larger airways and are associated with conditions like chronic bronchitis, bronchiectasis, and severe pulmonary edema. They are louder, lower-pitched, and may be heard throughout inspiration and sometimes expiration.
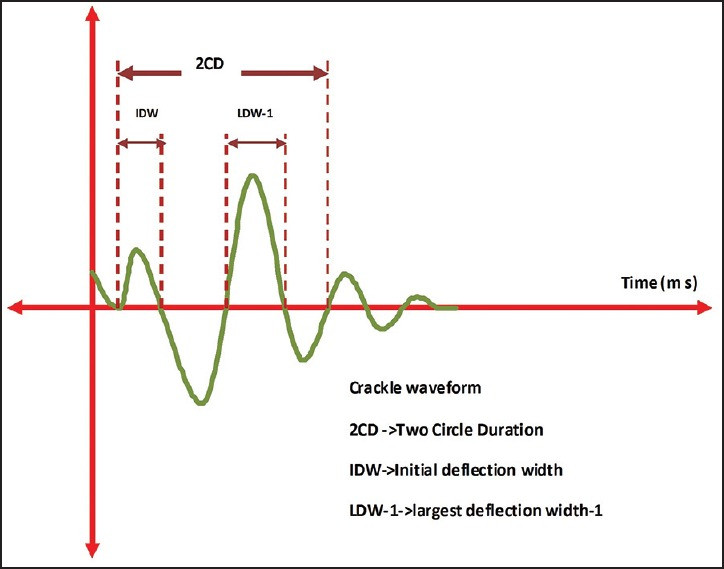 Figure 7
Figure 7
Crackles in Specific Conditions:
- COPD: Early inspiratory, coarse crackles, often heard at the mouth, indicating proximal airway involvement.
- Bronchiectasis: Early to mid-inspiratory, coarse crackles, heard throughout the chest, reduced by coughing.
- Idiopathic Pulmonary Fibrosis (IPF): Late inspiratory, fine “Velcro” crackles, predominantly at the bases, progressing upwards as the disease advances.
- Pneumonia: Mid-inspiratory coarse crackles in acute phase, becoming late inspiratory and finer during resolution.
- Heart Failure: Late inspiratory coarse crackles, typically basal, but can become pan-inspiratory in severe pulmonary edema.
Wheezes: Generalized or Focal, Expiratory or Inspiratory
Wheezes are continuous, musical, high-pitched sounds caused by airway narrowing.
Where to Listen:
- Generalized Wheezes (Polyphonic): Heard throughout the chest, common in asthma and COPD due to widespread airway obstruction. Auscultate over all lung fields, anteriorly and posteriorly.
- Focal Wheezes (Monophonic): Localized to a specific area, suggesting localized obstruction (e.g., tumor, foreign body). Focus auscultation on the affected region as indicated by history and other findings. Can be heard anteriorly, posteriorly, or laterally depending on the location of the obstruction.
Characteristics:
- High-pitched, musical quality, often described as whistling.
- Most commonly expiratory, but can be inspiratory or biphasic depending on the location and severity of obstruction.
- Louder than breath sounds and may be audible at the mouth or over the trachea.
Wheezes in Specific Conditions:
- Asthma and COPD: Polyphonic, expiratory wheezes heard diffusely.
- Localized Obstruction (Tumor, Foreign Body): Monophonic wheezes localized to the affected area.
Pleural Rub: Anterior and Lateral Chest Walls
Pleural rubs are grating, rubbing, or leathery sounds caused by inflammation of the pleural surfaces.
Where to Listen: Pleural rubs are best heard in areas where pleural inflammation is present, often along the anterior and lateral chest walls, where lung movement against the chest wall is most pronounced.
Characteristics:
- Non-musical, grating or rubbing sound.
- Heard during both inspiration and expiration, with the expiratory component mirroring the inspiratory component.
- May sound close to the ear and can be differentiated from crackles by their location, timing, and quality.
Differentiating Pleural Rub from Crackles:
| Feature | Pleural Rub | Crackles |
|---|---|---|
| Timing | Both inspiration and expiration | Primarily inspiration |
| Quality | Grating, leathery, rubbing | Discontinuous, explosive, non-musical |
| Effect of Cough | Not significantly altered | May be altered or disappear with cough |
| Location | Anterior and lateral chest walls | Varies; bases or throughout lungs |
Stridor: Primarily Over the Neck
Stridor is a loud, high-pitched, musical sound indicative of upper airway obstruction.
Where to Listen: Stridor is loudest over the neck (trachea) but can also be heard in the chest.
Characteristics:
- Loud, high-pitched, musical sound.
- Predominantly inspiratory in extrathoracic obstruction (e.g., laryngomalacia).
- Expiratory or biphasic in intrathoracic obstruction (e.g., tracheomalacia).
Stridor is a critical sign of airway compromise requiring prompt evaluation and management.
Vocal Resonance (Voice Sounds): Assessing Sound Transmission
Vocal resonance assesses the transmission of voice sounds through the lung tissue.
Where to Listen: Auscultate symmetrical locations across all lung fields while the patient speaks.
Types of Vocal Resonance:
- Bronchophony: Increased clarity and intensity of spoken words (“ninety-nine”) indicating consolidation.
- Whispered Pectoriloquy: Clear and distinct whispered sounds (“one-two-three”) also indicating consolidation.
- Egophony: “Ee” sound transforming to “Ay” sound, suggesting consolidation or pleural effusion. Auscultate areas where consolidation or effusion is suspected.
Other Auscultatory Signs and Locations
- Coin Test: For pneumothorax, bullae, hydropneumothorax. Place coin below mid-clavicle anteriorly and listen posteriorly at the same point.
- Scratch Test: For pneumothorax. Stethoscope on manubrium, scratch chest wall laterally, louder sound on pneumothorax side.
- Hippocratic Succussion Splash: For hydropneumothorax. Shake patient side-to-side and listen over area of air-fluid level.
- Hamman’s Sign (Mediastinal Crunch): For pneumomediastinum, pneumothorax. Listen over precordium (3rd-5th intercostal spaces) for crunching sound synchronous with heartbeat.
- Forced Expiratory Time (FET): Over suprasternal notch. Listen for duration of forced expiration.
- d’Espine’s Sign: Over spinous processes of upper thoracic vertebrae. Compare sound intensity to lateral lung sounds, increased intensity over vertebrae suggests mediastinal lymphadenopathy.
- Auscultatory Percussion: Tap manubrium, auscultate posterior thorax to assess resonance, useful for nodules, infiltrates, effusions.
Conclusion: Integrating Auscultation Location into Clinical Practice
Mastering lung auscultation involves not only recognizing different breath and adventitious sounds but also knowing where to listen for them most effectively. By systematically auscultating the anterior, posterior, and lateral chest walls, and by understanding the typical locations of normal and abnormal sounds, clinicians can significantly enhance their diagnostic accuracy. Integrating this knowledge into routine physical examinations will improve the detection and management of a wide range of respiratory conditions, ultimately benefiting patient care.
References
(References are the same as in the original article and are thus omitted here for brevity, as per instructions.)
